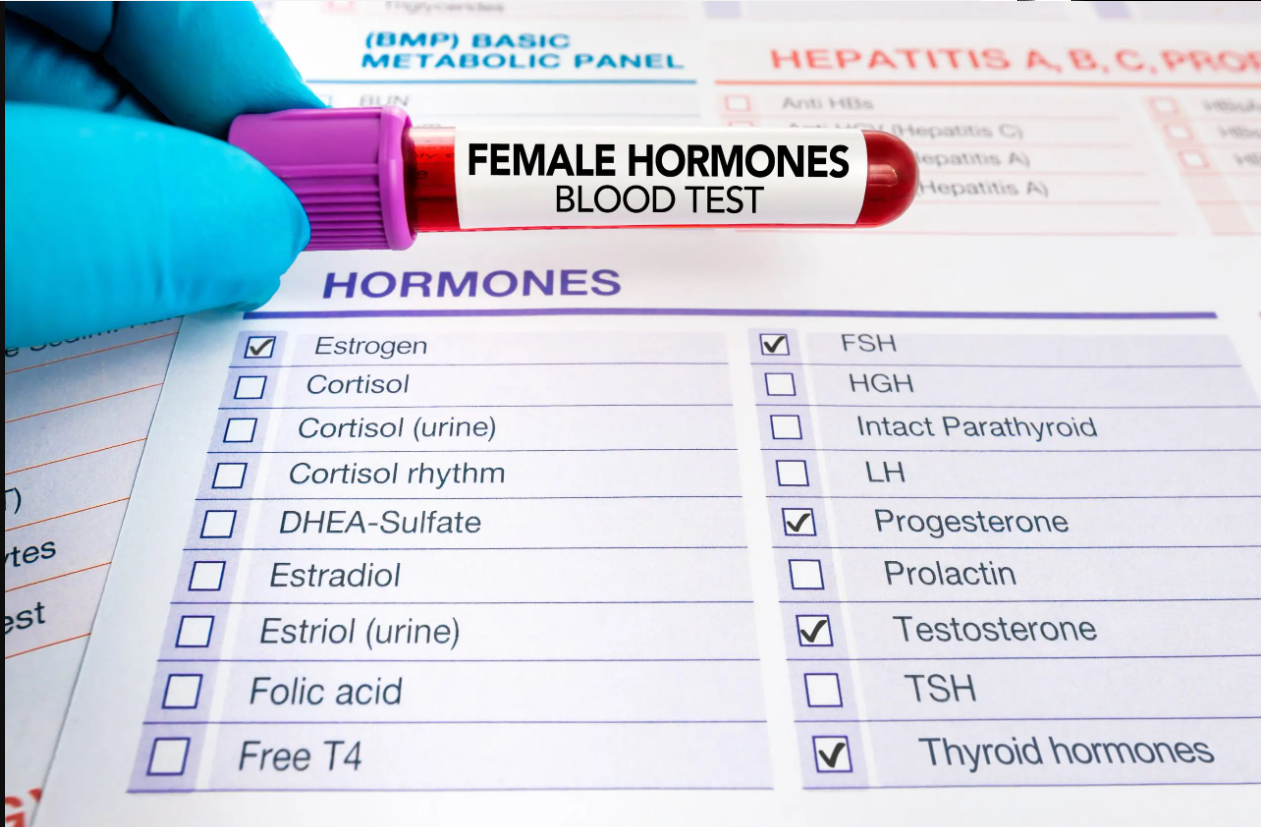
Women’s Hormone Tests
(LH, FSH, Estrogen, and Progesterone)
and Their Applications
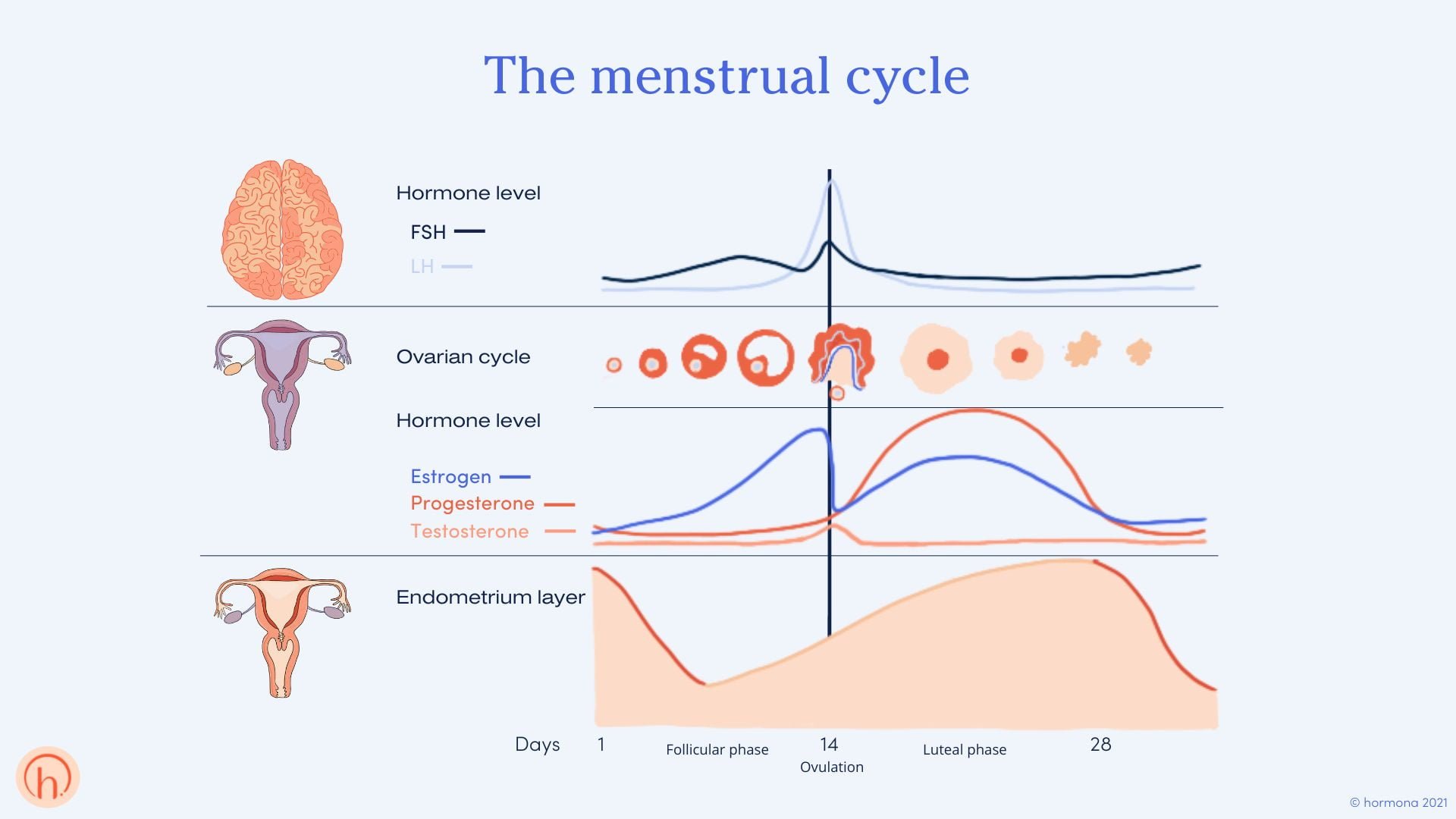
Hormones serve as the biochemical regulators of the female reproductive system, governing a diverse array of physiological processes. These include menstrual cycle modulation, folliculogenesis, ovulation, implantation, pregnancy maintenance, and menopausal transition. Each of these processes is intricately linked to endocrine signaling pathways that ensure reproductive function and systemic homeostasis. Among the most clinically relevant hormones in female endocrinology are Luteinizing Hormone (LH), Follicle-Stimulating Hormone (FSH), Estrogen (primarily estradiol), and Progesterone. These hormones not only govern reproductive function but also exert systemic effects on bone density, cardiovascular health, and metabolic processes. The precise measurement of these hormonal markers is imperative for diagnosing endocrine dysfunctions, optimizing fertility management, and formulating targeted therapeutic strategies. This article provides an in-depth analysis of these hormones, their physiological roles, clinical implications, and their diagnostic applications in contemporary medical practice.
Luteinizing Hormone (LH)
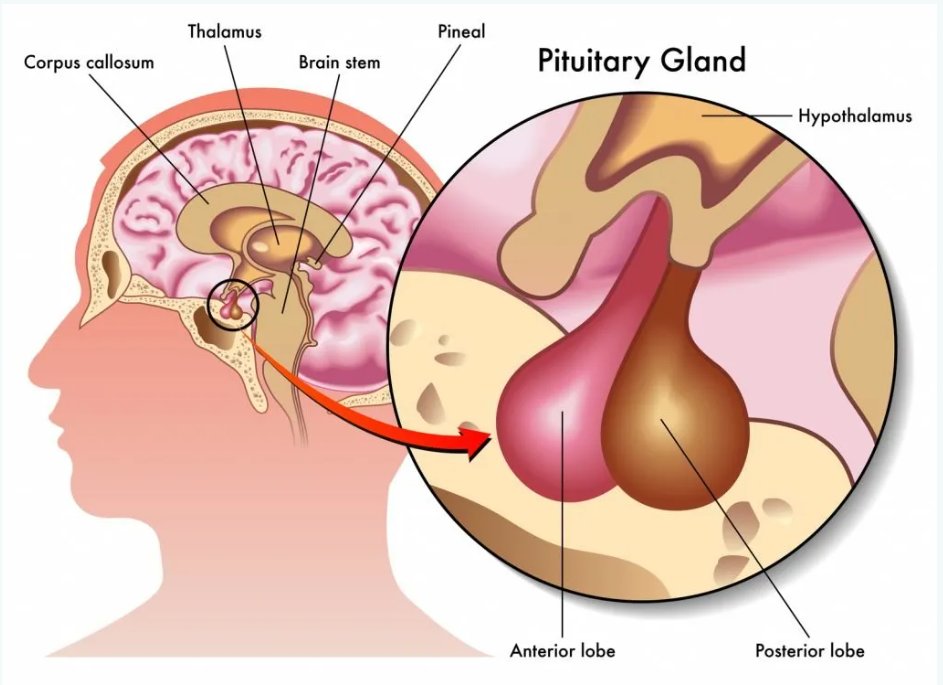
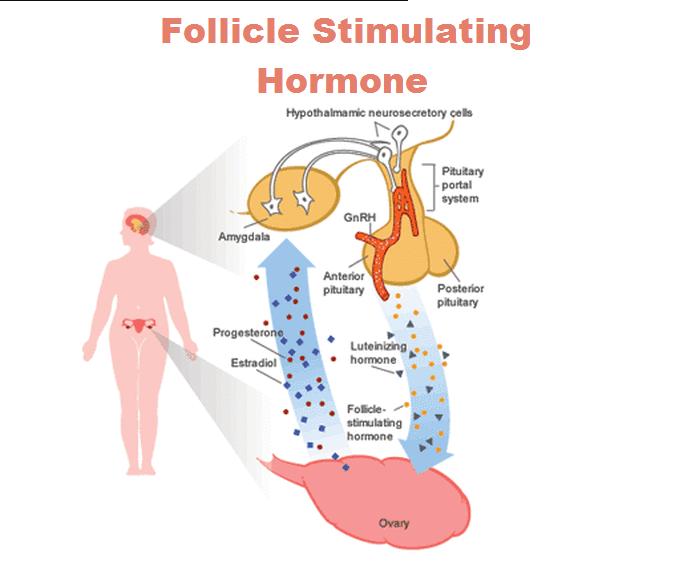
LH, a glycoprotein hormone secreted by the anterior pituitary, is indispensable for ovulation and corpus luteum function. It works in concert with FSH to regulate follicular development, with FSH promoting follicular growth and LH initiating ovulation through the LH surge. Additionally, LH plays a pivotal role in stimulating theca cells to produce androgens, which are subsequently converted to estrogens by granulosa cells under the influence of FSH. The feedback loops between LH, estrogen, and progesterone ensure the precise hormonal balance necessary for reproductive health. It operates within the hypothalamic-pituitary-ovarian (HPO) axis, where its pulsatile secretion is regulated by gonadotropin-releasing hormone (GnRH) and modulated through negative and positive feedback mechanisms by estrogen and progesterone.
Physiological Functions of LH
- Induction of ovulation via the LH surge, which triggers follicular rupture and the subsequent release of the oocyte.
- Promotion of luteinization of granulosa cells, leading to progesterone synthesis post-ovulation.
- Regulation of theca cell function, thereby facilitating androgen synthesis, a precursor to estrogen biosynthesis.
Clinical Applications of LH Testing
- Fertility and Ovulatory Dysfunction: LH measurement is critical in diagnosing polycystic ovary syndrome (PCOS), hypothalamic amenorrhea, and luteal phase deficiencies.
- Ovulation Prediction: LH surge detection is widely employed in ovulation predictor kits to optimize conception timing.
- Menopausal Transition Evaluation: Persistent elevation of LH levels, in conjunction with FSH, serves as an indicator of ovarian senescence.
- Hormonal Imbalance Investigation: Abnormal LH/FSH ratios are instrumental in diagnosing conditions such as gonadal dysgenesis and functional hypothalamic amenorrhea.
Follicle-Stimulating Hormone (FSH)
FSH, another anterior pituitary gonadotropin, orchestrates follicular recruitment and maturation while synergistically interacting with LH to regulate ovarian steroidogenesis.
Physiological Functions of FSH
- Induction of follicular growth by stimulating granulosa cell proliferation.
- Upregulation of aromatase enzyme activity, essential for estradiol biosynthesis from androgens.
- Enhancement of follicular dominance through modulation of FSH receptor expression, which directly influences follicular selection and subsequent ovulatory potential. Increased receptor sensitivity to FSH promotes the maturation of a dominant follicle, thereby optimizing conditions for successful ovulation and increasing the likelihood of conception.
Clinical Applications of FSH Testing
- Assessment of Ovarian Reserve: Elevated basal FSH levels correlate with diminished ovarian reserve and primary ovarian insufficiency (POI).
- Menstrual Irregularities Diagnosis: FSH testing aids in distinguishing primary ovarian failure from secondary (hypothalamic or pituitary) causes of amenorrhea.
- Menopause Confirmation: A persistently elevated FSH level (typically >30-40 IU/L) is diagnostic of menopause.
- PCOS Differentiation: Unlike primary ovarian failure, PCOS often presents with normal or low FSH relative to LH.
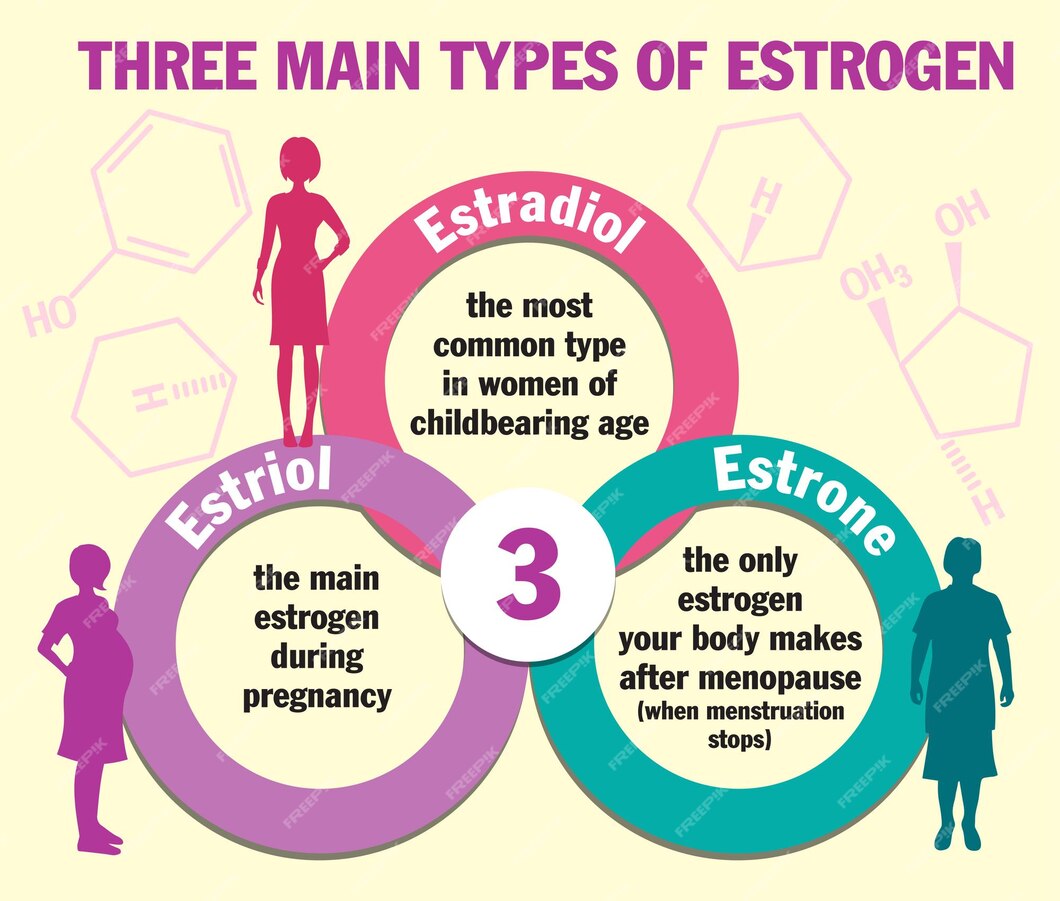
Estrogen (Estradiol, Estrone, Estriol)
Estrogens, particularly estradiol (E2), function as pivotal mediators of female reproductive physiology and broader systemic homeostasis.
Physiological Functions of Estrogen
- Regulation of endometrial proliferation, priming the uterus for implantation.
- Modulation of gonadotropin release via feedback loops within the HPO axis.
- Preservation of bone mineral density by inhibiting osteoclastic activity. In postmenopausal women, estrogen deficiency leads to increased bone resorption, significantly elevating the risk of osteoporosis and fractures. This underscores the critical role of estrogen in maintaining skeletal integrity and highlights the importance of hormonal assessments in osteoporosis risk evaluation and management.
- Maintenance of cardiovascular homeostasis through lipid profile regulation and endothelial function.
Clinical Applications of Estrogen Testing
- Evaluation of Hypogonadism: Low estradiol levels are indicative of ovarian dysfunction or central hypogonadotropic hypogonadism.
- Assessment of Menstrual and Ovulatory Disorders: Estrogen profiling is critical in cases of anovulation, abnormal uterine bleeding, and hypoestrogenic states.
- Hormone Replacement Therapy (HRT) Monitoring: Regular assessment ensures appropriate dosing in menopausal or post-oophorectomy patients.
- Bone Health Assessment: Chronic estrogen deficiency is a well-established risk factor for osteoporosis and increased fracture susceptibility.
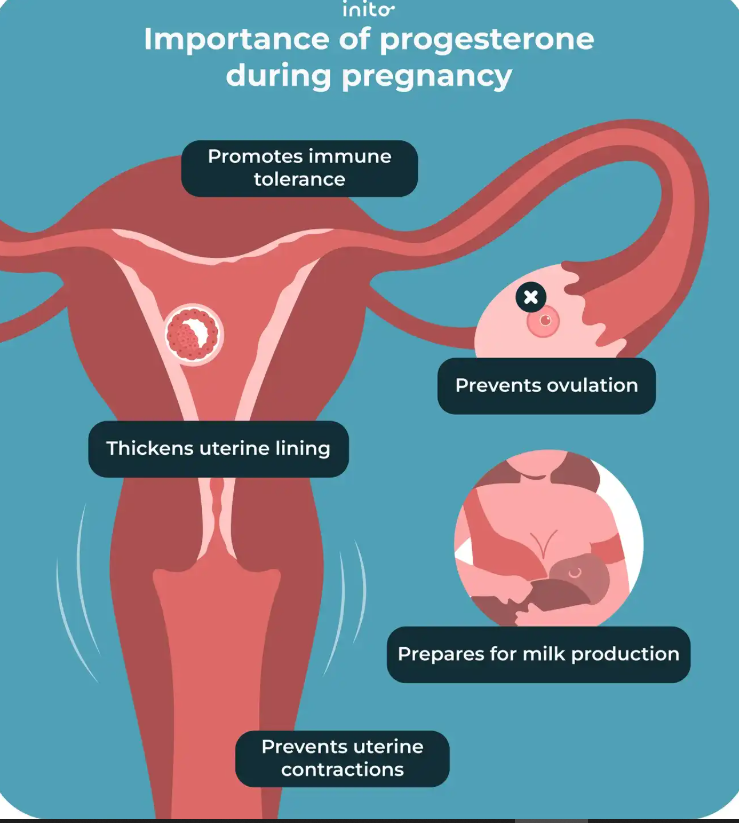
Progesterone
Progesterone, synthesized predominantly by the corpus luteum and later by the placenta during pregnancy, is essential for sustaining reproductive and systemic functions.
Physiological Functions of Progesterone
- Transformation of the endometrium into a secretory phase, conducive to embryo implantation.
- Inhibition of myometrial contractions, preventing premature expulsion of the conceptus.
- Immunomodulation to facilitate maternal-fetal tolerance.
- Regulation of thermogenic effects, often manifesting as a mid-luteal phase basal body temperature rise.
Clinical Applications of Progesterone Testing
- Ovulation Confirmation: Mid-luteal progesterone assessment is a reliable indicator of ovulatory function.
- Fertility Workup: Luteal phase insufficiency, characterized by inadequate progesterone secretion, is a leading cause of implantation failure and recurrent miscarriage.
- Endocrine Disorder Diagnosis: Aberrant progesterone levels contribute to conditions such as endometrial hyperplasia, luteal phase defects, and hormone-sensitive malignancies.
- HRT and Assisted Reproductive Technology (ART) Monitoring: Progesterone supplementation protocols necessitate regular hormone level assessments.
Conclusion
The precise quantification of LH, FSH, estrogen, and progesterone levels represents an indispensable diagnostic tool in reproductive endocrinology. These hormonal biomarkers not only facilitate the identification of ovulatory dysfunctions and ovarian pathologies but also provide essential data for therapeutic interventions in infertility, menstrual irregularities, and menopause management. The intricate crosstalk within the HPO axis underscores the necessity for a holistic and integrative approach to hormone testing. A multidisciplinary strategy, incorporating endocrinologists, reproductive specialists, and nutritionists, enhances diagnostic precision and treatment efficacy. For instance, in cases of infertility, a combined approach leveraging hormonal assays, metabolic assessments, and lifestyle interventions can significantly improve patient outcomes. ensuring that clinical decisions are informed by comprehensive endocrine profiling. As advancements in molecular endocrinology and precision medicine continue to evolve, the role of these hormonal assays in individualized patient care is poised to expand, fostering enhanced diagnostic accuracy and optimized reproductive health outcomes.