Reticulocyte Count: A Critical Biomarker of Erythropoietic Activity
The reticulocyte count serves as a fundamental hematologic parameter for evaluating erythropoietic activity and bone marrow functionality. Compared to other hematologic indices such as hemoglobin concentration, mean corpuscular volume (MCV), and erythropoietin levels, reticulocyte count offers a more direct measure of marrow erythroid output.
While hemoglobin and hematocrit levels reflect the overall oxygen-carrying capacity, they do not provide immediate insight into bone marrow responsiveness. Similarly, MCV can suggest underlying causes of anemia but lacks the dynamic nature of reticulocyte enumeration. In contrast, reticulocyte count, particularly when adjusted using the reticulocyte production index (RPI), provides a near-real-time assessment of erythropoietic activity, making it a superior marker for evaluating bone marrow function in both normal and pathological states.
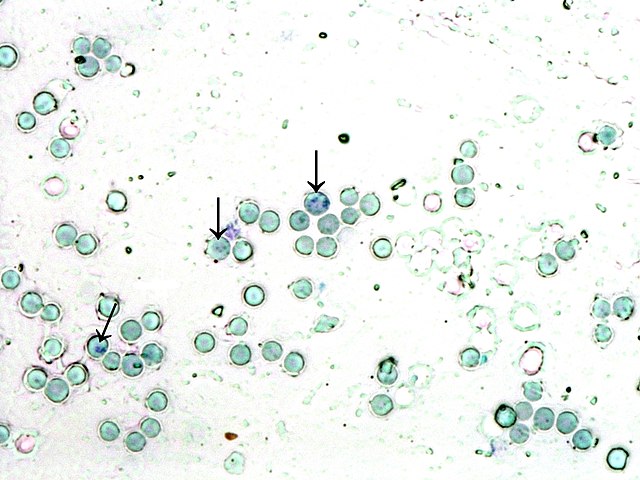
Reticulocytes, as nascent erythroid cells, retain residual ribosomal RNA, rendering them identifiable via supravital staining techniques. This assay provides a dynamic assessment of erythropoietic turnover, facilitating the diagnosis and monitoring of diverse hematological pathologies. Given its sensitivity to alterations in erythropoiesis, reticulocyte enumeration is frequently employed in both clinical and research settings to assess hematopoietic homeostasis and dysregulation.
Physiological and Pathophysiological Roles of Reticulocytes
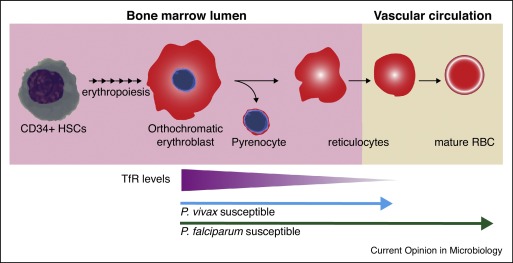
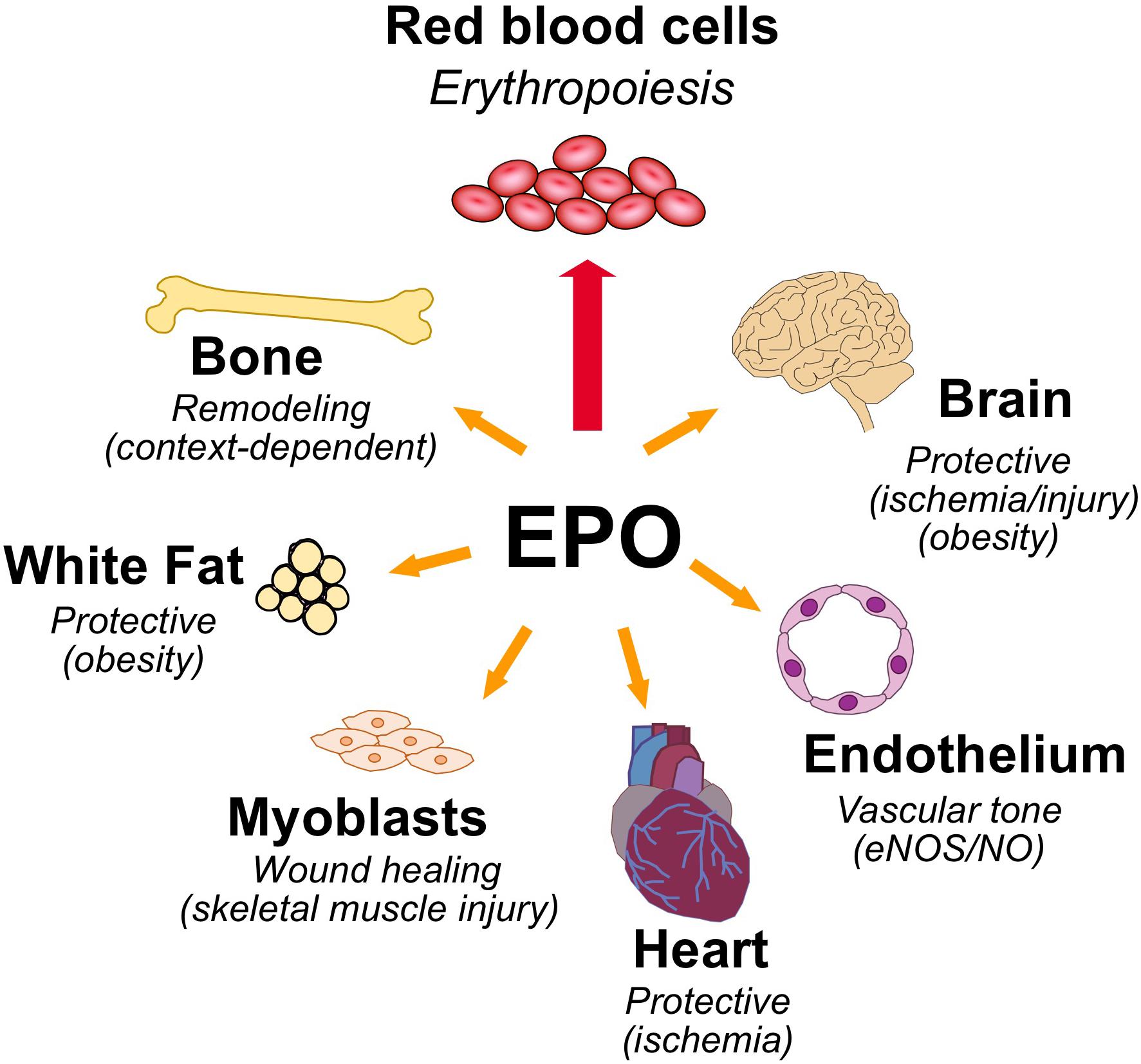
Reticulocytes represent an intermediary stage in erythroid differentiation, transitioning from normoblasts to mature erythrocytes within the peripheral circulation. The reticulocyte maturation process, which spans 24 to 48 hours, is critical for optimal hemoglobinization and membrane remodeling. This process is tightly regulated by erythropoietin (EPO), which modulates erythroid progenitor proliferation and differentiation.
The proportion of circulating reticulocytes serves as an index of bone marrow responsiveness to both physiological demands and pathophysiological stressors. In states of erythropoietic hyperactivity, such as hemolysis or acute hemorrhage, reticulocytosis reflects a compensatory increase in marrow output. Conversely, reticulocytopenia suggests impaired erythropoiesis due to bone marrow dysfunction or erythropoietin insufficiency.
Clinical Applications of Reticulocyte Quantification
Reticulocyte enumeration is integral to the diagnostic and prognostic evaluation of several hematological disorders. The ability to distinguish between different etiologies of anemia and bone marrow failure syndromes is particularly crucial in guiding clinical management.
Some of the primary applications include:
Characterization and Differentiation of Anemia:
- Elevated reticulocyte indices denote heightened erythropoietic compensation in response to acute blood loss or hemolytic anemias. In these cases, the bone marrow exhibits robust regenerative capacity, as evidenced by an increased absolute reticulocyte count.
- Conversely, suppressed reticulocytosis suggests inadequate erythropoietic drive, commonly observed in bone marrow suppression, nutrient deficiencies (e.g., iron, cobalamin, folate), or chronic disease states such as anemia of chronic inflammation (ACI). A persistently low reticulocyte count in the presence of anemia warrants further investigation into marrow pathology or systemic factors inhibiting erythropoiesis.
Surveillance of Bone Marrow Recovery:
- Serial reticulocyte measurements provide insight into post-chemotherapy marrow reconstitution, hematopoietic stem cell engraftment, and recovery from aplastic anemia. An increasing reticulocyte count following bone marrow suppression signifies hematopoietic recovery and is often used as a prognostic marker in post-transplant settings.
Optimization of Erythropoiesis-Stimulating Agent (ESA) Therapy:
- Patients with erythropoietin-deficient states, such as chronic kidney disease (CKD), undergo ESA therapy, where reticulocyte trends serve as a biomarker for therapeutic efficacy and dose adjustments. Insufficient reticulocytosis despite ESA therapy may indicate functional iron deficiency or inadequate dosing, necessitating further intervention.
Evaluation of Hemolytic Disorders:
- In hemolytic anemias—including autoimmune hemolysis, sickle cell disease, and hereditary spherocytosis—reticulocytosis is a hallmark compensatory response to premature erythrocyte destruction. A disproportionately high reticulocyte count relative to hemoglobin levels may indicate ongoing hemolysis and necessitate further diagnostic workup, including direct antiglobulin tests (DAT) and hemolysis markers such as lactate dehydrogenase (LDH) and haptoglobin.
Assessment of Bone Marrow Suppression and Infiltration:
- Conditions such as myelodysplastic syndromes (MDS), leukemia, and metastatic cancer infiltration of the bone marrow often manifest with reticulocytopenia due to ineffective hematopoiesis. In these disorders, reticulocyte count findings are often integrated with bone marrow biopsy and genetic testing to refine diagnosis and assess disease severity. Bone marrow biopsy provides histopathological confirmation of marrow infiltration, dysplasia, or fibrosis, while genetic analysis can detect clonal hematopoiesis or specific mutations (e.g., TP53, JAK2, SF3B1) that influence prognosis and treatment strategies. Combining these diagnostic modalities enables a more comprehensive evaluation of erythropoietic dysfunction, guiding therapeutic decisions such as bone marrow transplantation or targeted therapies. In these settings, reticulocyte counts, when interpreted alongside bone marrow biopsy findings, contribute to diagnostic precision and prognostication.
Analytical Considerations in Reticulocyte Enumeration
Reticulocyte quantification is expressed through multiple indices, each offering distinct clinical insights:
- Absolute Reticulocyte Count (ARC): The total concentration of reticulocytes per microliter of blood, offering an absolute measure of erythropoietic activity. This parameter is particularly useful in distinguishing hypoproliferative anemias from those with adequate marrow compensatory responses.
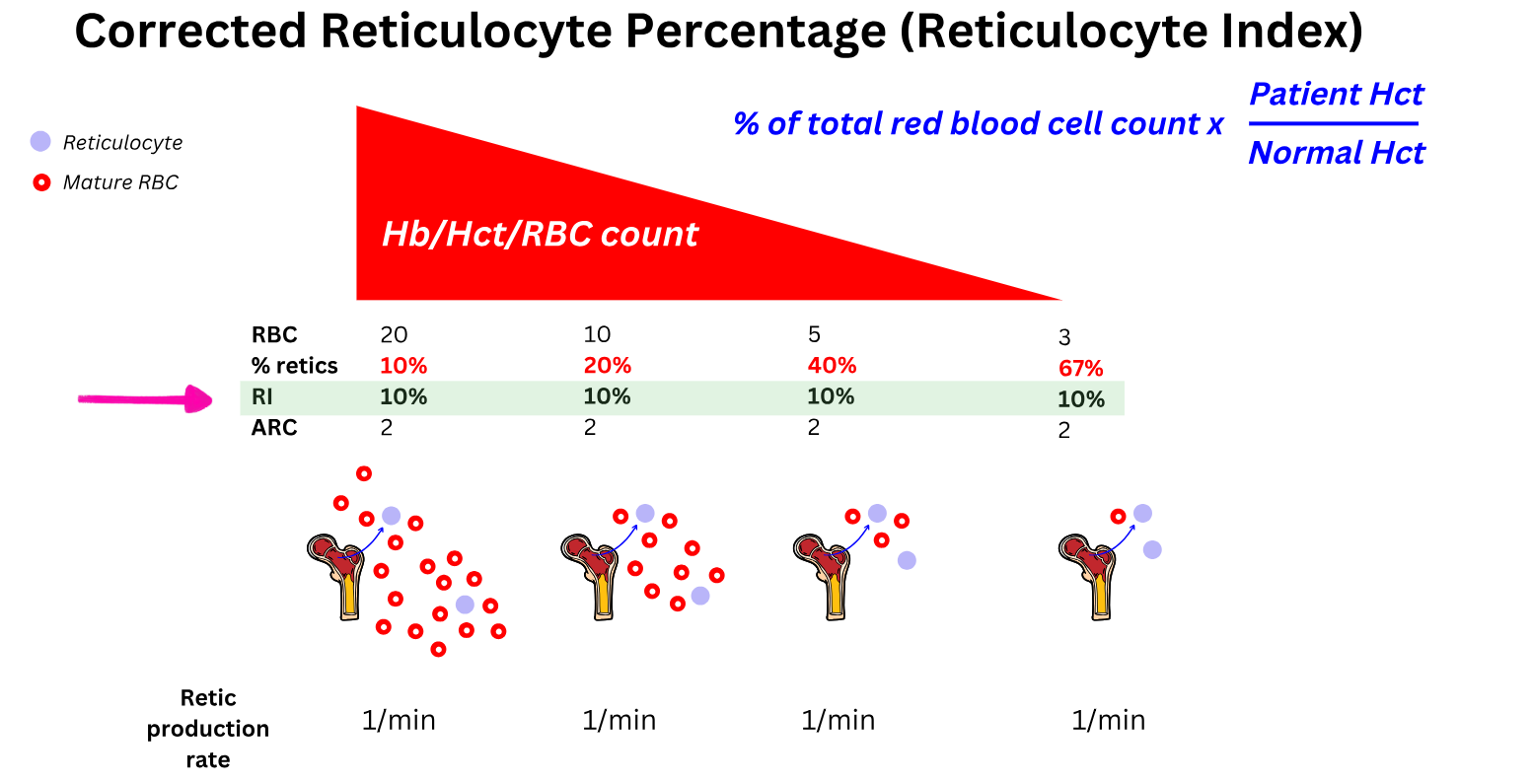
- Reticulocyte Percentage: The proportion of reticulocytes relative to total erythrocytes, which requires correction for anemic states to yield clinically meaningful interpretations. A raw percentage may be misleading in cases of severe anemia, where the total erythrocyte count is markedly reduced.
To enhance diagnostic accuracy, the Reticulocyte Production Index (RPI) is often employed, normalizing the reticulocyte percentage for anemia severity and marrow maturation time, thus providing a refined assessment of erythropoietic kinetics.

where the maturation correction factor adjusts for the prolonged circulation time of reticulocytes in anemia. This correction ensures that the reticulocyte response is accurately interpreted relative to the severity of anemia, allowing for a more precise assessment of bone marrow activity. This index adjusts for the extended lifespan of reticulocytes in circulation in cases of anemia, offering a more accurate representation of marrow responsiveness.
Determinants Influencing Reticulocyte Count
Several endogenous and exogenous factors modulate reticulocyte kinetics, necessitating careful interpretation of results. In a clinical setting, these factors can be differentiated through a combination of laboratory assessments, patient history, and diagnostic imaging. For example, nutritional deficiencies such as iron, vitamin B12, and folate insufficiencies can be confirmed through serum assays, whereas myelosuppressive therapy effects can be correlated with treatment history and bone marrow biopsy findings. Chronic inflammatory states are often identified via inflammatory markers like C-reactive protein (CRP) and interleukin-6 (IL-6), while pharmacologic influences require medication review and temporal association analysis. By integrating these assessments, clinicians can more precisely attribute changes in reticulocyte count to their underlying causes, enhancing diagnostic accuracy and treatment planning.
- Nutritional status: Deficiencies in essential erythropoietic substrates, including iron, vitamin B12, and folate, can impair reticulocyte production, often preceding overt anemia.
- Myelosuppressive therapies: Cytotoxic chemotherapy and radiation therapy induce transient marrow suppression, often resulting in a decline in reticulocyte counts.
- Chronic inflammatory states: Pro-inflammatory cytokines, particularly interleukin-6 (IL-6), can suppress erythropoiesis via hepcidin-mediated iron sequestration, leading to anemia of chronic inflammation with concomitant reticulocytopenia.
- Pharmacologic influences: Certain medications, including immunosuppressants, corticosteroids, and erythropoiesis-stimulating agents, can modulate reticulocyte dynamics, necessitating context-specific evaluation.
- Bone marrow fibrosis and infiltration: Disorders such as primary myelofibrosis or metastatic malignancies may result in bone marrow failure, leading to persistently low reticulocyte counts despite anemia.
Conclusion
Reticulocyte quantification constitutes a pivotal diagnostic and prognostic tool in hematology, providing a real-time reflection of erythropoietic dynamics. Its utility extends from anemia characterization to therapeutic monitoring and marrow function assessment. The integration of absolute and corrected reticulocyte indices enhances clinical decision-making, allowing for nuanced differentiation of erythropoietic insufficiency versus hyperactivity. Given its broad clinical applicability, ongoing advancements in automated reticulocyte analysis and flow cytometric methodologies are poised to further refine the precision and diagnostic yield of this essential hematologic parameter. Emerging technologies, such as high-throughput flow cytometry with multi-parametric gating, allow for more precise differentiation of reticulocyte subpopulations. Additionally, novel RNA-based assays and machine learning algorithms are being integrated into reticulocyte analysis, enhancing the detection of subtle hematopoietic abnormalities. These advancements not only improve diagnostic accuracy but also offer potential for earlier intervention in hematologic disorders.