Practical Guide to Preparing for Medical Lab Tests
Medical laboratory tests are essential for accurately diagnosing, monitoring, and preventing a broad spectrum of diseases and disorders. These assessments furnish clinicians with critical biochemical, hematological, microbiological, and imaging data necessary for informed medical decision-making. The precision of test results is contingent upon meticulous patient preparation, which minimizes pre-analytical variability and enhances diagnostic reliability. This guide elucidates essential preparatory protocols for common laboratory investigations to optimize clinical outcomes.
1. Understanding the Scope and Purpose of Laboratory Testing
A comprehensive understanding of the rationale behind specific diagnostic tests is fundamental for both healthcare providers and patients. Laboratory assessments encompass multiple domains, including but not limited to:
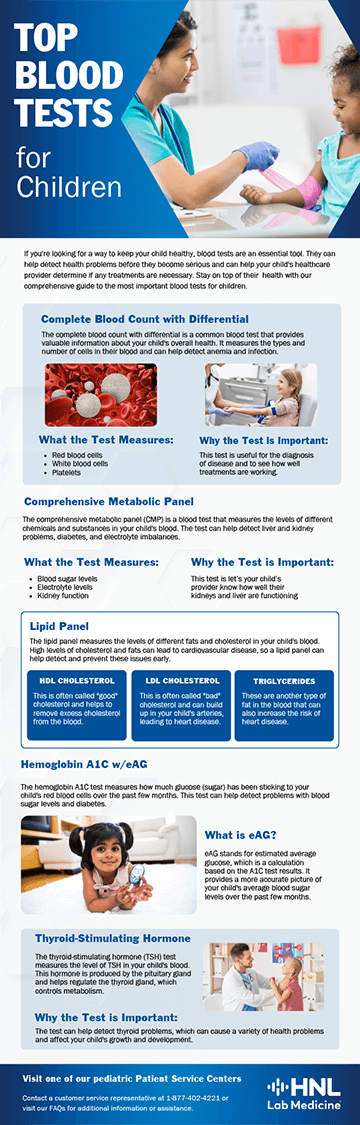
- Hematological Analyses – Complete blood count (CBC), coagulation panels, and peripheral blood smears.
- Biochemical and Metabolic Panels – Lipid profiles, glucose tolerance tests, renal and hepatic function assessments.
- Endocrinological Evaluations – Thyroid function panels, reproductive hormone assays, and adrenal function tests.
- Microbiological and Infectious Disease Diagnostics – Bacterial, viral, fungal, and parasitic cultures, serologies, and polymerase chain reaction (PCR) assays.
- Immunological and Autoimmune Panels – Antinuclear antibody (ANA) testing, rheumatoid factor (RF) assays, and immunoglobulin profiling.
A thorough discussion with the ordering physician regarding the necessity, methodology, and implications of the prescribed test(s) is advised.
2. Fasting and Dietary Restrictions
Fasting is a critical preparatory requirement for several biochemical and metabolic evaluations, ensuring the accuracy of parameters such as glucose, lipids, and enzymatic activity. Common tests necessitating fasting include:
- Fasting Plasma Glucose and Oral Glucose Tolerance Test (OGTT) – A minimum of 8-12 hours of fasting is required.
- Lipid Panel (Cholesterol and Triglycerides Assessment) – A fasting period of 9-12 hours optimizes lipid fraction accuracy.
- Comprehensive Metabolic Panel (CMP) and Liver Function Tests – Fasting facilitates precise enzymatic and electrolyte measurements.
During the fasting period, patients must abstain from caloric intake, including solid foods, beverages other than water, chewing gum, and tobacco use, as these can significantly alter metabolic readouts. Tobacco consumption, particularly nicotine, can influence catecholamine release, leading to fluctuations in blood glucose and lipid metabolism, which may compromise the accuracy of fasting-dependent tests.
3. Pharmacological Considerations and Supplementary Intake
Exogenous substances, including prescription medications, over-the-counter drugs, herbal remedies, and nutritional supplements, may interfere with laboratory assays. It is imperative to:
- Consult with a healthcare provider regarding the temporary discontinuation or adjustment of medications prior to testing.
- Disclose all pharmacological agents, including anticoagulants, corticosteroids, hormonal therapies, and nephrotoxic drugs, to the laboratory personnel.
- Avoid unnecessary self-administration of vitamins and supplements that could skew test results, particularly biotin (which affects thyroid and cardiac biomarker assays).
4. Hydration, Dietary Patterns, and Lifestyle Modifications
- Optimal Hydration – Adequate water intake enhances venous access for phlebotomy and ensures proper urine concentration for renal function evaluation.
- Dietary Moderation – The avoidance of excessive fatty, sugary, and protein-heavy meals prior to testing is essential, as dietary composition can transiently influence metabolic markers.
- Alcohol and Caffeine Avoidance – Ethanol consumption alters hepatic enzyme activity, while caffeine can modify stress hormone levels and cardiac parameters.
5. Timing and Biological Rhythms in Sample Collection
Certain laboratory tests exhibit diurnal variations, necessitating precise timing for optimal accuracy:
- Morning Collections – Cortisol, testosterone, and fasting glucose levels are optimally measured in early morning hours due to their circadian fluctuations.
- Serial and Timed Sampling – Therapeutic drug monitoring (TDM) and postprandial glucose evaluations require strict adherence to predefined intervals.
- Home-Based Specimen Collection – Patients collecting urine, stool, or saliva samples must rigorously adhere to handling, storage, and transport protocols to preserve sample integrity.
6. Mitigation of Physiological and Psychological Stressors
Stress-induced physiological alterations can impact hormone assays, inflammatory markers, and cardiovascular metrics by triggering the hypothalamic-pituitary-adrenal (HPA) axis and sympathetic nervous system activation. This response elevates cortisol levels, alters cytokine production, and affects hemodynamic parameters, potentially leading to misleading laboratory results. Recommendations include:
- Minimizing Psychological Stress – Patients should engage in relaxation techniques prior to testing to avoid transient hypercortisolemia and autonomic nervous system activation.
- Avoiding Strenuous Physical Activity – Intensive exercise can acutely affect creatine kinase (CK), lactate, and glucose levels, potentially confounding laboratory interpretation.
7. Considerations for Reproductive and Female-Specific Tests
- Menstrual Cycle Timing – Hormonal assessments, including estradiol, progesterone, and luteinizing hormone (LH), should be scheduled based on the phase of the menstrual cycle.
- Pregnancy Adjustments – Pregnancy status must be communicated to clinicians as it significantly alters metabolic, hematological, and hormonal baselines.
- Fertility and Reproductive Assessments – Ovarian reserve testing (AMH, FSH) and semen analysis require stringent pre-test guidelines.
8. Procedural Expectations During Sample Collection
- Venipuncture and Capillary Blood Sampling – Patients should expect minor discomfort and potential hematoma formation post-procedure.
- Urinalysis and Microbiological Cultures – Midstream clean-catch urine samples reduce contamination risks; sterile techniques are imperative for bacterial cultures.
- Saliva, Buccal Swabs, and Genetic Testing – Patients should refrain from food and beverage intake for a designated period before sample collection to ensure accuracy.
9. Post-Test Protocols and Follow-Up Care
- Post-Fasting Nutritional Recovery – Light meals post-testing help in stabilizing blood glucose and energy levels.
- Monitoring Adverse Reactions – Patients should report dizziness, prolonged bleeding, or adverse reactions following venipuncture.
- Consulting Physicians for Data Interpretation – A thorough review of laboratory findings with a healthcare provider facilitates appropriate medical intervention and follow-up diagnostics if necessary.
Conclusion
The accuracy of medical laboratory diagnostics depends on thorough pre-analytical preparation, which minimizes errors and ensures reliable test results. Stringent adherence to fasting protocols, pharmacological disclosures, hydration guidelines, and test-specific directives is paramount for ensuring the clinical validity of results. A heightened awareness of physiological variability, stress modulation, and test-specific scheduling further enhances diagnostic precision. By rigorously following these preparatory guidelines, patients and healthcare professionals can collaboratively optimize the utility of laboratory investigations, leading to more accurate diagnoses and improved patient care outcomes.