LDL, HDL, and Triglycerides:
Advanced Insights into Cholesterol and Lipid Metabolism
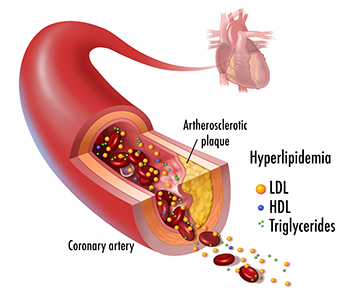
Cholesterol and lipid metabolism play a fundamental role in human physiology, influencing multiple critical processes. These include cell membrane composition, steroidogenesis, and bile acid synthesis, all of which contribute to metabolic homeostasis. Despite its essential roles, dyslipidemia—an imbalance in lipid levels—represents a critical determinant of atherosclerotic cardiovascular disease (ASCVD), metabolic syndrome, and other systemic disorders. This article provides an in-depth exploration of Low-Density Lipoprotein (LDL), High-Density Lipoprotein (HDL), and triglycerides, delineating their molecular characteristics, pathophysiological implications, diagnostic considerations, and interventional strategies.
Biochemical Mechanisms Underpinning Lipid Transport
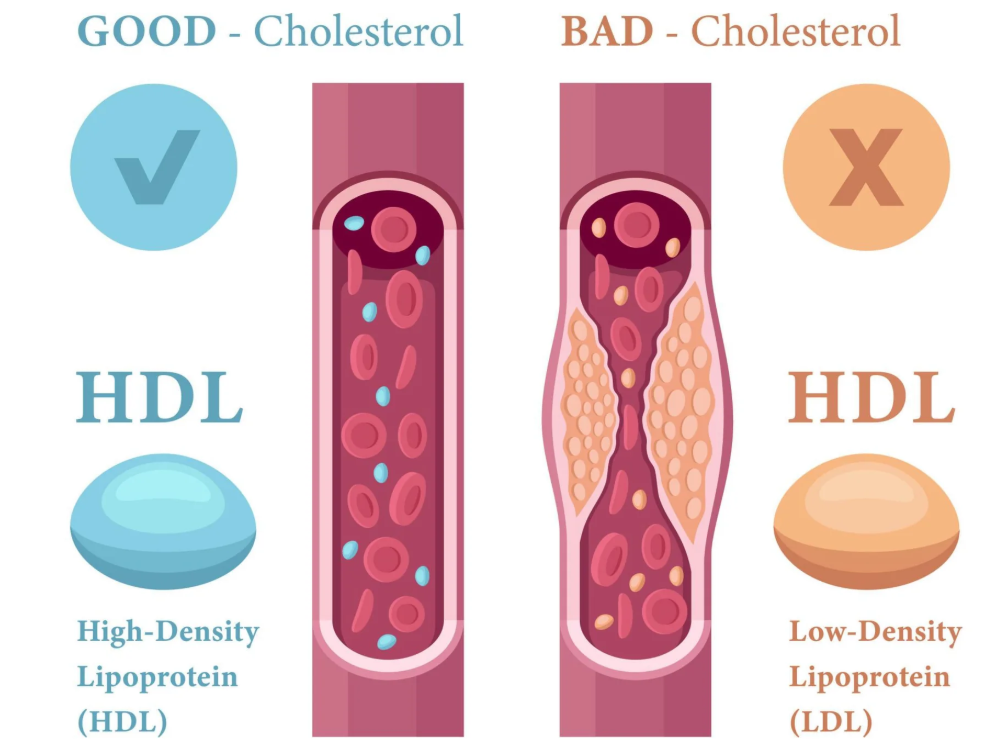
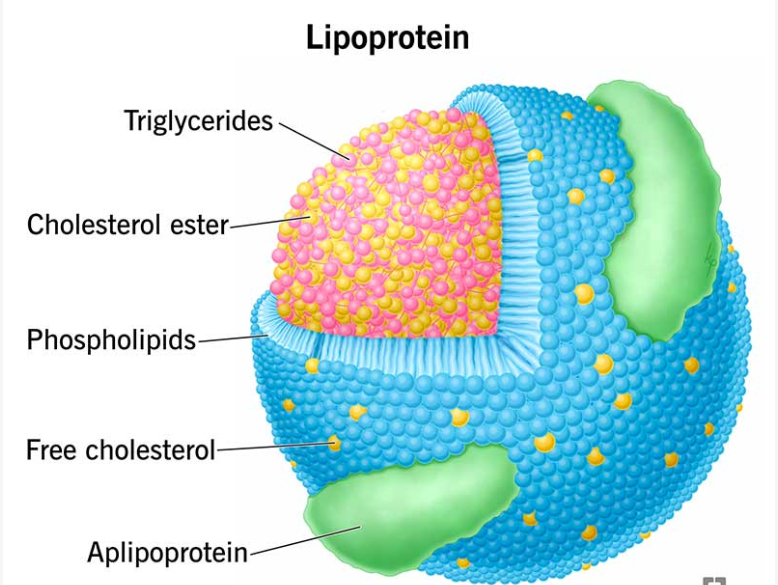
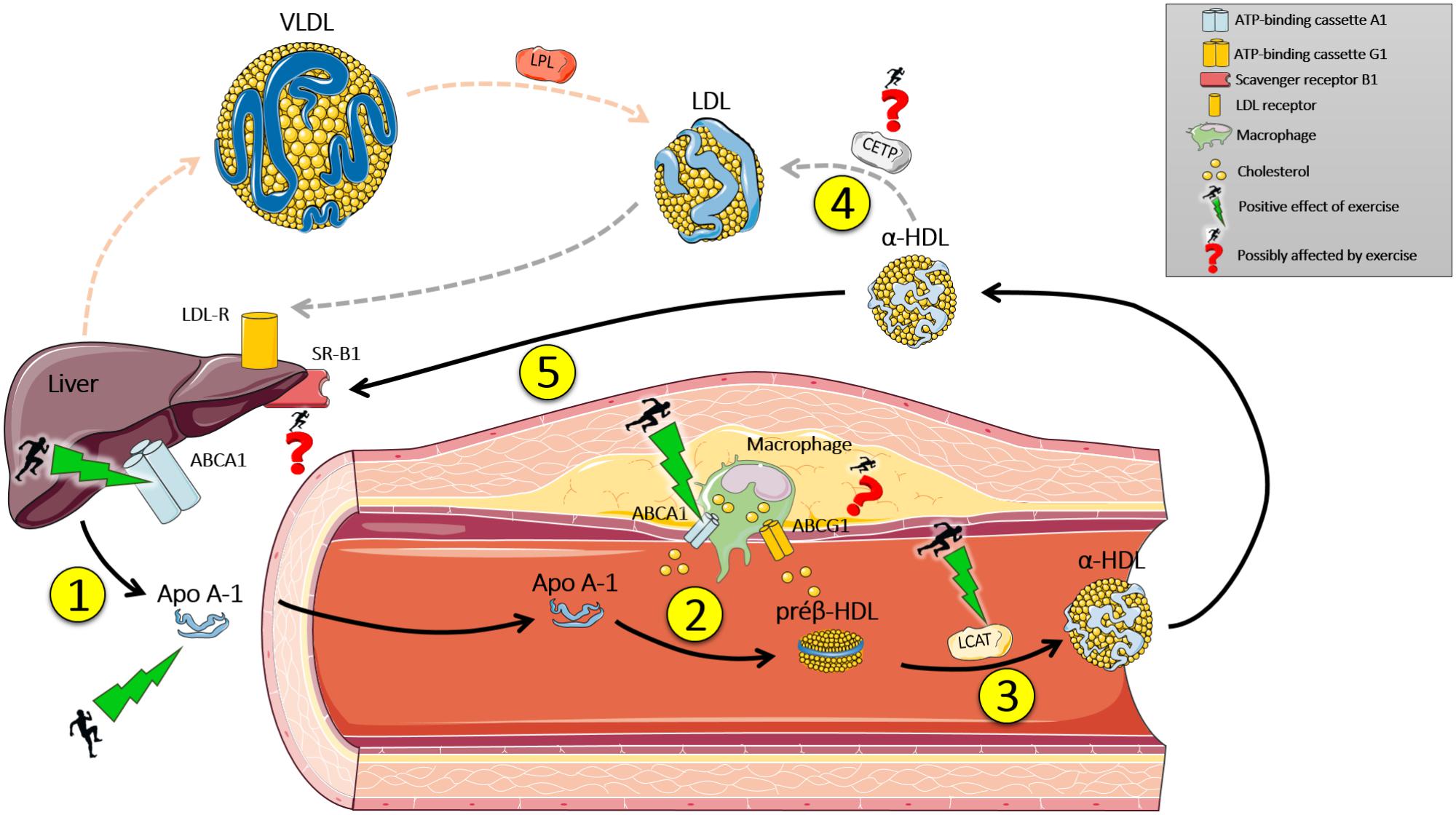
Cholesterol, inherently hydrophobic, necessitates a sophisticated transport system via lipoproteins, which function as macromolecular vehicles composed of apolipoproteins, phospholipids, and a lipid core. The dynamic interplay between LDL and HDL orchestrates lipid trafficking, with LDL primarily mediating cholesterol delivery to peripheral tissues, while HDL facilitates reverse cholesterol transport to the liver for biliary excretion. These processes are tightly regulated by hepatic and extrahepatic mechanisms, ensuring lipid homeostasis.
LDL (Low-Density Lipoprotein):
Atherogenic Potential and Molecular Pathophysiology
LDL is a predominant carrier of plasma cholesterol, playing a crucial role in maintaining cellular membrane integrity by regulating cholesterol availability, which influences membrane fluidity and functionality. Additionally, LDL provides cholesterol essential for steroid hormone synthesis, supporting endocrine functions. However, elevated LDL concentrations predispose individuals to oxidative modifications, leading to macrophage foam cell formation, endothelial dysfunction, and arterial plaque development. These mechanisms underpin atherogenesis, the hallmark of coronary artery disease (CAD) and ischemic events.
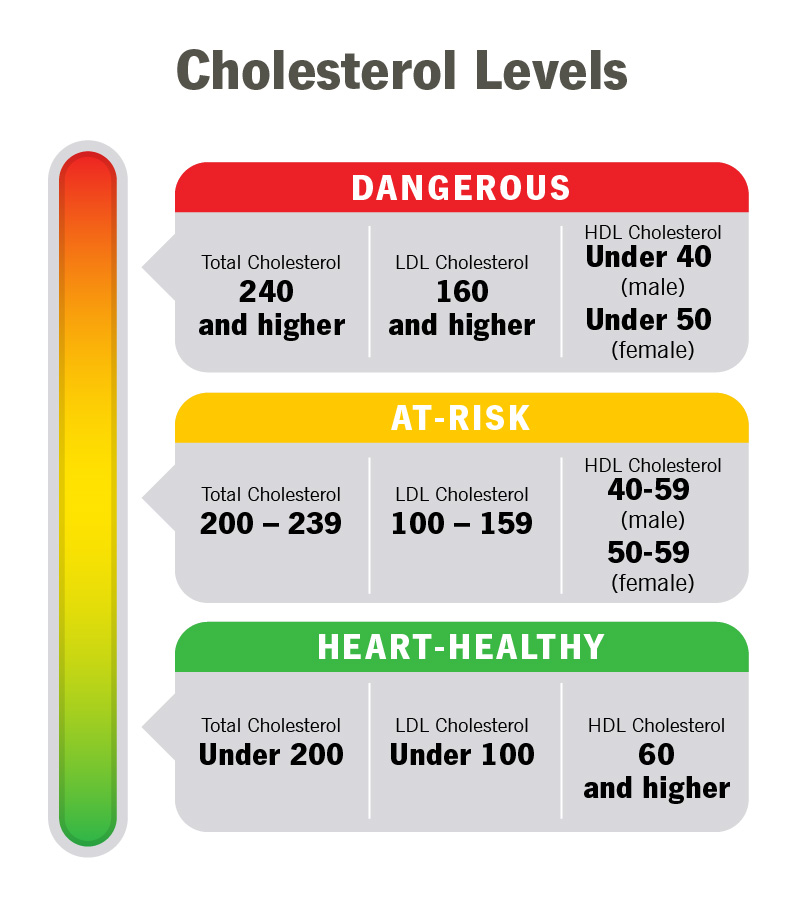
Clinical Reference Ranges for LDL Cholesterol:
- Optimal: <100 mg/dL
- Near Optimal: 100-129 mg/dL
- Borderline High: 130-159 mg/dL
- High: 160-189 mg/dL
- Very High: ≥190 mg/dL
Targeted Therapeutic Strategies for LDL Reduction:
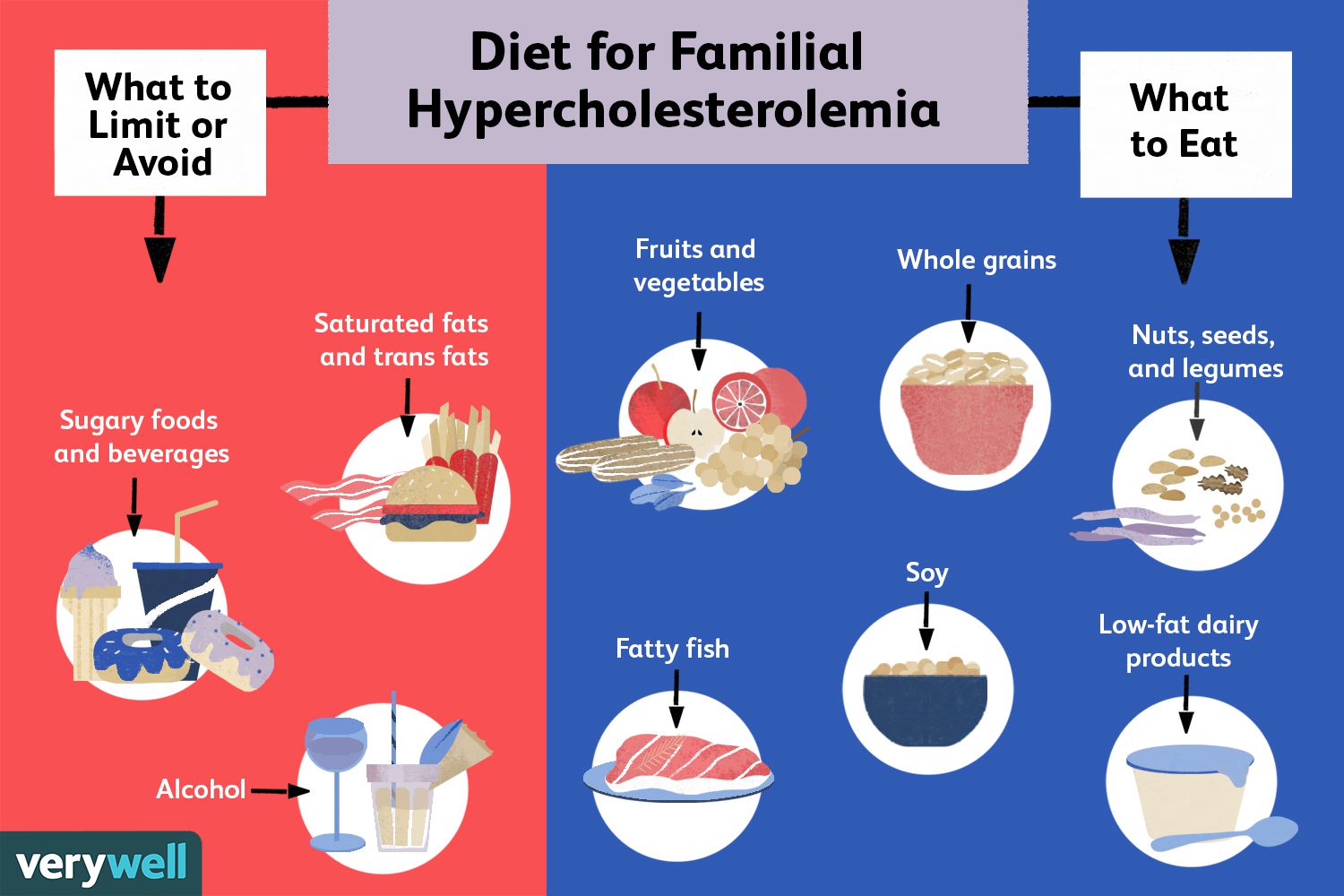
- Dietary Modulation: Emphasis on monounsaturated fats, polyunsaturated fats, and dietary fiber
- Pharmacological Interventions: Statins (HMG-CoA reductase inhibitors), PCSK9 inhibitors, bile acid sequestrants, and ezetimibe
- Lifestyle Modifications: Structured aerobic exercise, weight optimization, and cessation of tobacco products
HDL (High-Density Lipoprotein):
Cardioprotective Properties and Clinical Relevance
HDL is pivotal in reverse cholesterol transport (RCT), a process in which excess cholesterol is extracted from peripheral tissues and conveyed to the liver for excretion. Beyond cholesterol efflux, HDL exerts antioxidative, anti-inflammatory, and endothelial-protective effects, rendering it a crucial factor in cardiovascular risk mitigation.
Clinical Reference Ranges for HDL Cholesterol:
- Low (Increased Cardiovascular Risk): <40 mg/dL (men), <50 mg/dL (women)
- Intermediate: 40-59 mg/dL
- High (Cardioprotective): ≥60 mg/dL
Strategies for HDL Augmentation:
- Nutritional Optimization: Omega-3 fatty acids, polyphenols, and phytosterols
- Physical Activity: High-intensity interval training (HIIT) and resistance training
- Lifestyle Adjustments: Cessation of tobacco use, moderated alcohol consumption, and improved sleep hygiene
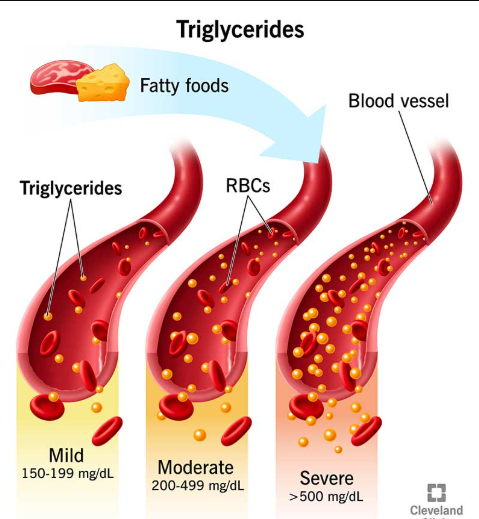
Triglycerides: Metabolic Significance and Clinical Implications
Triglycerides serve as a primary energy reservoir, stored in adipose tissue as lipid droplets and mobilized through lipolysis when energy demands increase. Under hormonal regulation—primarily by insulin, glucagon, and catecholamines—triglycerides are hydrolyzed into free fatty acids and glycerol, which are subsequently utilized for ATP production via β-oxidation in mitochondria. Their regulation is intricately linked to metabolic homeostasis, with dysregulation contributing to insulin resistance, hepatic steatosis, and cardiovascular disease risk. Hypertriglyceridemia is frequently associated with insulin resistance, metabolic syndrome, and an increased propensity for pancreatitis. Additionally, emerging research suggests a strong correlation between elevated triglyceride levels and residual ASCVD risk, independent of LDL cholesterol.
Clinical Reference Ranges for Triglycerides:
- Normal: <150 mg/dL
- Borderline High: 150-199 mg/dL
- High: 200-499 mg/dL
- Very High: ≥500 mg/dL
Interventional Approaches for Triglyceride Modulation:
- Dietary Interventions: Restriction of refined carbohydrates, fructose, and saturated fats
- Pharmacotherapy: Fibrates, omega-3 fatty acid supplements, and niacin
- Exercise and Weight Management: Reduction of visceral adiposity and engagement in structured aerobic activity
Lipid Panel Interpretation and Advanced Biomarker Assessment
A standard lipid panel comprises total cholesterol, LDL, HDL, and triglycerides, as these markers collectively provide a comprehensive assessment of lipid metabolism and cardiovascular risk. Total cholesterol serves as a general indicator of lipid levels, while LDL is the primary atherogenic factor associated with plaque formation. HDL is measured for its protective role in reverse cholesterol transport, and triglycerides reflect metabolic status and energy utilization. Together, these markers aid in diagnosing dyslipidemia and guiding therapeutic interventions. However, the refinement of cardiovascular risk stratification necessitates adjunctive biomarkers, including:
- Apolipoprotein B (ApoB): A superior predictor of atherogenic lipoprotein burden
- LDL Particle Size and Number: Small dense LDL particles exhibit heightened atherogenic potential
- Lipoprotein(a) [Lp(a)]: An independent risk factor for coronary artery disease
Evidence-Based Lifestyle and Nutritional Modifications for Optimal Lipid Profiles
- Dietary Patterns: Adoption of Mediterranean and Dietary Approaches to Stop Hypertension (DASH) dietary models
- Physical Activity Recommendations: Minimum of 150 minutes per week of moderate-to-vigorous aerobic activity, coupled with resistance training
- Obesity and Lipid Dysregulation: Targeted weight reduction strategies for individuals with metabolic syndrome
- Smoking and Alcohol Consumption: Avoidance of tobacco products and moderation of alcohol intake
- Stress Management: Implementation of mindfulness-based stress reduction (MBSR) techniques to mitigate dyslipidemic responses
Emerging Therapeutic Frontiers in Lipid Management
Recent advancements in lipid-lowering therapies have introduced novel pharmacological agents with unprecedented efficacy in cholesterol modulation. These include:
- Inclisiran: A small interfering RNA (siRNA) therapy targeting PCSK9 mRNA, reducing LDL receptor degradation
- Bempedoic Acid: An ATP citrate lyase inhibitor that attenuates cholesterol biosynthesis upstream of HMG-CoA reductase
- Angiopoietin-like Protein 3 (ANGPTL3) Inhibitors: Novel agents that reduce triglyceride-rich lipoproteins
Conclusion and Future Directions
LDL, HDL, and triglycerides serve as pivotal determinants of lipid homeostasis and cardiovascular pathology. While traditional lipid metrics remain central to risk stratification, emerging biomarkers and novel pharmacotherapeutics offer enhanced precision in dyslipidemia management. Future research endeavors will likely elucidate the genetic and epigenetic underpinnings of lipid metabolism, with a particular focus on gene-environment interactions, lipidomic profiling, and novel regulatory pathways influencing cholesterol synthesis and clearance. Advances in CRISPR-based gene editing, RNA-based therapeutics, and microbiome-lipid interactions are promising areas that could revolutionize personalized lipid-lowering strategies. Additionally, a deeper understanding of lipid metabolism in diverse populations may help tailor interventions to specific genetic backgrounds, reducing disparities in cardiovascular outcomes. By integrating evidence-based lifestyle interventions, pharmacological advancements, and precision medicine, clinicians can optimize cardiovascular risk reduction and improve long-term patient outcomes.